Human preliminaries will start inescapably – yet regardless of whether they work out positively and a fix is found, there are numerous hindrances before worldwide vaccination is plausible
Indeed, even at their best – and draconian – control systems have just eased back the spread of the respiratory malady Covid-19. With the World Health Organization at long last proclaiming a pandemic, everyone’s eyes have gone to the possibility of an antibody, in light of the fact that solitary an immunization can keep individuals from becoming ill.
Around 35 organizations and scholastic foundations are hustling to make such an antibody, at any rate four of which as of now have up-and-comers they have been trying in creatures. The first of these – created by Boston-based biotech firm Moderna – will enter human preliminaries quickly.
This extraordinary speed is thanks in huge part to early Chinese endeavors to succession the hereditary material of Sars-CoV-2, the infection that causes Covid-19. China shared that succession toward the beginning of January, permitting research bunches the world over to develop the live infection and study how it attacks human cells and makes individuals wiped out.
In any case, there is another purpose behind the head start. Despite the fact that no one could have anticipated that the following irresistible ailment to undermine the globe would be brought about by a coronavirus – influenza is commonly considered to represent the best pandemic hazard – vaccinologists had supported their wagers by taking a shot at “model” pathogens. “The speed with which we have [produced these candidates] constructs especially on the interest in seeing how to create immunizations for different coronaviruses,” says Richard Hatchett, CEO of the Oslo-based charitable the Coalition for Epidemic Preparedness Innovations (Cepi), which is driving endeavors to back and arrange Covid-19 antibody advancement.

Coronaviruses have caused two other ongoing plagues – extreme intense respiratory disorder (Sars) in China in 2002-04, and Middle East respiratory disorder (Mers), which began in Saudi Arabia in 2012. In the two cases, work started on immunizations that were later racked when the episodes were contained. One organization, Maryland-based Novavax, has now repurposed those antibodies for Sars-CoV-2, and says it has a few applicants prepared to enter human preliminaries this spring. Moderna, in the mean time, based on prior work on the Mers infection led at the US National Institute of Allergy and Infectious Diseases in Bethesda, Maryland.
Sars-CoV-2 offers somewhere in the range of 80% and 90% of its hereditary material with the infection that caused Sars – consequently its name. Both comprise of a portion of ribonucleic corrosive (RNA) inside a circular protein case that is shrouded in spikes. The spikes lock on to receptors on the outside of cells covering the human lung – a similar kind of receptor in the two cases – permitting the infection to break into the phone. Once inside, it captures the cell’s regenerative apparatus to deliver more duplicates of itself, before breaking out of the cell again and murdering it simultaneously.
All immunizations work as indicated by a similar essential standard. They present part or the entirety of the pathogen to the human resistant framework, ordinarily as an infusion and at a low portion, to provoke the framework to deliver antibodies to the pathogen. Antibodies are a sort of resistant memory which, having been inspired once, can be immediately assembled again if the individual is presented to the infection in its regular structure.

Generally, inoculation has been accomplished utilizing live, debilitated types of the infection, or part or entire of the infection once it has been inactivated by warmth or synthetic substances. These strategies have disadvantages. The live structure can keep on advancing in the host, for instance, possibly recovering a portion of its destructiveness and making the beneficiary wiped out, while higher or rehash dosages of the inactivated infection are required to accomplish the important level of security. A portion of the Covid-19 immunization ventures are utilizing these attempted and-tried methodologies, yet others are utilizing more current innovation. One later system – the one that Novavax is utilizing, for instance – builds a “recombinant” immunization. This includes removing the hereditary code for the protein spike on the outside of Sars-CoV-2, which is the piece of the infection well on the way to incite an insusceptible response in people, and gluing it into the genome of a bacterium or yeast – driving these microorganisms to produce enormous amounts of the protein. Different methodologies, even more up to date, sidestep the protein and construct immunizations from the hereditary guidance itself. This is the situation for Moderna and another Boston organization, CureVac, the two of which are building Covid-19 immunizations out of errand person RNA.
Cepi’s unique arrangement of four supported Covid-19 immunization ventures was vigorously slanted towards these progressively imaginative innovations, and a week ago it reported $4.4m (£3.4m) of organization financing with Novavax and with a University of Oxford vectored antibody venture. “Our involvement in antibody improvement is that you can’t envision where you’re going to stagger,” says Hatchett, implying that decent variety is critical. Furthermore, the phase where any methodology is well on the way to falter is clinical or human preliminaries, which, for a portion of the applicants, are going to get going.
Clinical preliminaries, a basic forerunner to administrative endorsement, as a rule occur in three stages. The first, including two or three dozen solid volunteers, tests the immunization for security, observing for antagonistic impacts. The second, including a few hundred individuals, for the most part in a piece of the world influenced by the illness, takes a gander at how powerful the immunization is, and the third does likewise in a few thousand individuals. Be that as it may, there’s a significant level of steady loss as exploratory immunizations go through these stages. “Not all ponies that leave the beginning entryway will complete the race,” says Bruce Gellin, who runs the worldwide inoculation program for the Washington DC-based philanthropic, the Sabin Vaccine Institute.
There are valid justifications for that. Either the up-and-comers are perilous, or they’re incapable, or both. Screening out duds is basic, which is the reason clinical preliminaries can’t be skipped or rushed. Endorsement can be quickened if controllers have affirmed comparative items previously. The yearly influenza immunization, for instance, is the result of an all around sharpened sequential construction system wherein just one or a couple of modules must be refreshed every year. Interestingly, Sars-CoV-2 is a novel pathogen in people, and huge numbers of the advances being utilized to construct antibodies are generally untested as well. No immunization produced using hereditary material – RNA or DNA – has been affirmed to date, for instance. So the Covid-19 antibody competitors must be treated as spic and span immunizations, and as Gellin says: “While there is a push to get things done as quick as could be expected under the circumstances, it’s extremely significant not to take alternate routes.”
An outline of that is an antibody that was created during the 1960s against respiratory syncytial infection, a typical infection that causes cold-like side effects in kids. In clinical preliminaries, this immunization was found to disturb those side effects in newborn children who proceeded to come down with the infection. A comparable impact was seen in creatures given an early trial Sars antibody. It was later adjusted to dispose of that issue be that as it may, since it has been repurposed for Sars-CoV-2, it should be gotten through particularly stringent security testing to preclude the danger of upgraded infection.
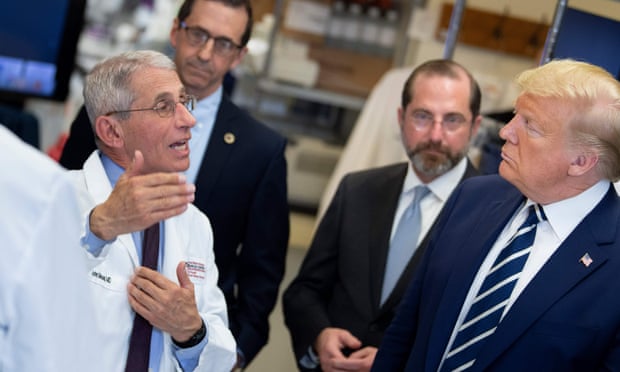
It’s thus that taking an immunization competitor right to administrative endorsement commonly takes 10 years or more, and why President Trump planted disarray when, at a gathering at the White House on 2 March, he squeezed for an antibody to be prepared by the US races in November – an incomprehensible cutoff time. “Like most vaccinologists, I don’t figure this antibody will be prepared before year and a half,” says Annelies Wilder-Smith, educator of rising irresistible sicknesses at the London School of Hygiene and Tropical Medicine. That is as of now very quick, and it accept there will be no hitches.
Meanwhile, there is another potential issue. When an antibody is endorsed, it will be required in huge amounts – and huge numbers of the associations in the Covid-19 immunization race basically don’t have the vital creation limit. Antibody improvement is now a dangerous undertaking, in business terms, in light of the fact that scarcely any competitors go anyplace close to the facility. Creation offices will in general be customized to explicit antibodies, and scaling these up when you don’t yet have a clue whether your item will succeed isn’t financially attainable. Cepi and comparable associations exist to bear a portion of the hazard, keeping organizations boosted to grow genuinely necessary antibodies. Cepi plans to put resources into building up a Covid-19 immunization and boosting fabricating limit in equal, and recently it put out a call for $2bn to permit it to do as such.
When a Covid-19 antibody has been endorsed, a further arrangement of difficulties will introduce itself. “Getting an antibody that is demonstrated to be protected and powerful in people takes one, best case scenario about 33% of the route to what’s required for a worldwide vaccination program,” says worldwide wellbeing master Jonathan Quick of Duke University in North Carolina, creator of The End of Epidemics (2018). “Infection science and antibodies innovation could be the restricting components, however legislative issues and financial aspects are undeniably bound to be the boundary to inoculation.”
The issue is ensuring the immunization finds a good pace who need it. This is a test even inside nations, and some have worked out rules. In the situation of an influenza pandemic, for instance, the UK would organize immunizing human services and social consideration laborers, alongside those considered at most elevated clinical hazard – including youngsters and pregnant ladies – with the general objective of keeping affliction and demise rates as low as would be prudent. In any case, in a pandemic, nations additionally need to contend with one another for medications.





























